COPD
Contact Us: 07957266649
Chronic
Obstructive
Pulmanory
Disorder
information for patients on COPD
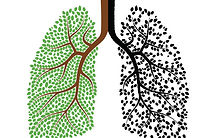
This page will show the anatomy of the lungs, then will show visually how COPD effects the anatomy and phisiology of the lungs. we will do this by comparing the lungs and airway of a healthy person with the lungs and airway of a COPD sufferer, i will explain the changes COPD has on the airway and lungs, later we will see how these changes in anatomy and phisiology effect the individual with COPD
anatomy & phisology
Emphysemia dierctly effects the alveoli it limits thier ability to expire air, causing the patient difficulty breathing out. the alveoli walls break down lossing elastic tissure and cologen therefore lossing thier elacsticity which contributes to expiration, the alveoli and air spaces distal to the terminal bronchioles become abnormally enlarged, the cappilary beds around the alveoli are also destroyed. this leads to a reduction in the surface area for gas exhange (west 2007).

healthy alveloi with cell walls intact, alveoli capable of increasing and decreasing in size, lots of surface area for gaseous ecchange.
unhealthy alveoli, cell walls destoryed incapable of contracting to failitate proper exhalation, less surface area and capillary bef for gaseous exhange.
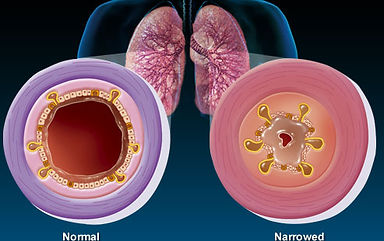
Chronic Bronchitus is when the mucosa memberances in the cell walls of the bronchi become inflamed recurant damage cause by irritant pollutants, this casues excess secreations of mucosa (sputum) which along with the inflamtion of the cell wall of the bronchi, there is a substantial deficit in airflow both too and from the alvoli for gaseous exhange (west 2007).

The lungs are part of the respiratory system, the main role of the respiratory system is maintaining homeostasis by providing the means for gas exchange between the atmospheric air and too blood and tissue (Tortora & Derrickson 2011). oxygen needs to exchange into the blood stream and then into cells as they are needed for metabolic reactions, at the same time these reactions release carbon dioxide, becuase co2 is acidic if it is allowed to build up in the body it can become toxic damaging cells.
For respiration to function properly the lungs need to inspire and expire successfully to do this the lungs need to create pressures inside of the organ which allows for the movement of air in and out. Negative pressure is need for inspiration this is achieved by the use of respiratory muscles which include the diaphragm, intercostal muscles and auxiliary respiratory muscles (Tortora & Derrickson 2011)which expand the thoracic cavity to creating negative pressure. Also the lungs are protected by a double layer serous membrane called the pleural membrane, which consists of superficial layer the parietal pleura and the deep layer the visceral pleura. The space in-between is the pleural cavity which contains lubricating fluid secreted by membranes; this allows the pleura to slide over each other with minimal friction. Plural fluid also causes the two membranes to adhere to one another which create surface tension (Marieb & Hoehn 2014) which keeps the lungs patent and aids the respiratory muscles by keeping the lungs attached to the thoracic cavity. Inside the alveolus surfactant is produced to lower surface tension of fluid within the alveoli (Marieb & Hoehn 2014) this lowered surface tension stops the alveoli from remaining closed upon expiration so maintains patency. positive pressure is requires upon expiration this is achieved by the elastic fibres that interconnect between alveoli and airways these as well as keeping airways and alveoli patent create a recoiling force that make the lungs recoil into a smaller shape that they are at full inhalation, surface tension within the alvoli also plays a part in creating positive pressure within the lungs (Marieb & Hoehn 2014). Although drastically reduced by the surfactant it still plays a part in recoiling the lungs back into there resting positions.
Inhaled air reaches the lungs through the mouth then the larynx it then passes through the trachea which is about 12cm long and 2.5 cm in diameter (Marieb & Hoehn 2011) it is located anterior to the oesophagus. The trachea has a thick wall which contains numerous layers, from deep to superficial they are the mucosa, submucosa, hyaline cartilage and the adventitia .The trachea is composed of 16 to 10 c shaped rings of hyaline cartilage (West 2007) these rings of cartilage provide a semi-ridged support for the trachea which maintains patency are connected together by dense connective tissue. a fibro muscular membrane spans the opening of the cartilage within this membrane are transverse muscle fibres called the trachealis muscles these allow the diameter of the trachea to change during inhalation and exhalation.
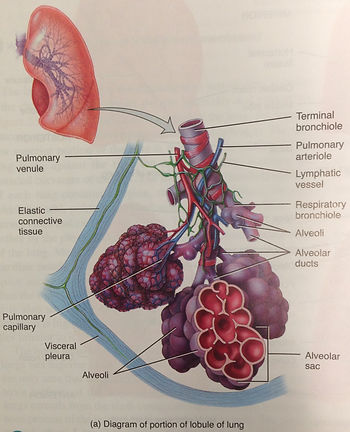
The trachea splits at the carina into two bronchus the the left primary bronchus nad the right primary bronchus which is more vertical (Marieb & Hoehn 2014), these primary bronchus divide further into the secondary (lobular bronci) there is one for each lobe of the lung with the right lungs having three lobes and the left two (Tortora & Derrickson 2011). The secondary lobular bronchi continue to branch forming smaller still bronchi called tertiary (segmental) bronchi each of which supplies a bronchopulmanory segment. These bronchi segment further into bronchioles. These bronchioles branch repeatedly eventually after enough divisions they branch into the smallest bronchioles which are terminal bronchioles. There are changes in the structure of the bronhi and bronchioles as they become more distal such as the amount of cartilage decreases and the amount of smooth muscle increases (Tortora & Derrickson 2011). Also the mucus membrane changes there are less goblet and muscosal producing cells in lower bronchioles with almost non present in terminal bronchioles (Tortora & Derrickson 2011).
Alveolar sacs and the alveoli themselves are found at the distal end of the terminal bronchioles. An alveolar sac consists of two or more alveoli that share a common opening (alveolar duct) . the alvoli themselves are a cup shaped opening lined by simple squamous epithelium and supported by a thin elastic membrane. the walls of the alveoli consist of two types of alveolar epithelial cells type 1 are simple squamous epithelium cells that form a nearly continuous lining of the alveolar wall these sites are the main sites for gas exchange along with the cappilarry wall they form the respiratory membrane which is very thin only 0.5um across (Marieb & Hoehn 2014) this thin enough for oxygen and carbon dioxide to diffuse across into red blood cells to be carried throughout the body. the second type of cell type 2 are rounded or cuboidal epithelium cells with free surfaces containing microvilli, these cells secrete fluid which contains amongst other things surfactant (Marieb & Hoehn 2014)which is important in lowering the surface tension of the alveolus fluid, which maintains the patency of the alveolus which reduces the chance of the alveoli collapsing.
healthy bronchioles, large airway with fully functioning mucosal glands and cillia. thin layer of mucus membrance.
a bronchiole suffereing from chronic bronchitits. inflamed epithelium cells casue swelling narrowing airways. increased mucosal production and damaged epithelium cells cause mucus buildup.
(Tortora J. Gerard & Derrickson Bryan 2011)
(Tortora J. Gerard & Derrickson Bryan 2011)
(WebMD.com 2014)
(Seplessons.ucsf.edu 2014)