COPD
Contact Us: 07957266649
Chronic
Obstructive
Pulmanory
Disorder
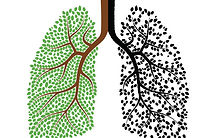
information for patients on COPD
Chronic bronchitis is characterised by a presence of cough & phlegm for more than 3 months of 2 consecutive years in the absence of other diseases recognised to cause sputum production.
Chronic bronchitis is caused by mainly by inhaling irritants into the lungs.
Causes include;
Causes lead to reduced amount of air passage via inflation and mucus production.
Irritants cause damage to the epithelium cells that line the airways, fluid swells in damaged tissue inflaming the cells and therefore narrowing the airways increasing airflow resistance.
Due to the irritation to the airways hypersecreation ( increased mucosal production) occurs in an attempt to clean the lungs.
-
Goblet cells increase in number and populate smaller airways.
-
Sub mucosal glands become enlarged (hypertrophy)
Because of the dual action of the inflamed tissue and the presence of more sputum the airways become narrowed which leads to increased airflow resistance which will result in difficulty to breath (Tillotson 2009).
In the early stages of chronic bronchitis the excess sputum does not yet completely obstruct the airways. the cough reflex is still functional as the lungs are still capable of expelling the mucus, also the mucus cannot yet become purulent.
Gradual paralysis of the cilia (Cilia are slender protuberances that project from the much larger cell body. the move in unison creating a wafting force capable of moving secretions) permits accumulation of mucus in smaller airways. Air can no longer be forced out of the lungs in great volume because of the small airways obstructions. (Barnett 2006) States that this makes coughing less effective so mucus cannot be effectively expectorated from the lungs.
"infalmation & irritation of airways causing airway narrowings"
chronic bronchitis
-
tobaco exposure, primary or secondary
-
deficiency of alpha-1 antitrypsin
-
occupational exposure
-
dusty envirments
-
pre exisiting broncial hyper-responsiveness
-
deficient diet
-
low birth weight
-
socioeconomic factors
-
childhood repiratory problems
Larger and Larger amounts of mucus are present in the airway, mucus begins to stagnate, bacteria can begin to colonise due to warm, dark, damp & stick environments. After the sputum has stagnated pulmonary infections become a lot more frequent.
Bacterial presence exacerbates mucus production ( Hass & Hass 2000), this leads to a detrimental cycle of infection which leads to increased mucus production which in turn leaves the lungs more susceptible to infection.
Smaller and Smaller airways are effected. Eventual peak excess of sputum leads to mucus presence in airways with crucial links to air sacks containing alveoli.
Little to no gas exchange happens in alveoli until secretions leave
With time obstruction of terminal & respiratory bronchioles becomes more widespread, mucus leaves at a slower rate.
Because of mucus build up in lower airways air can become trapped in alveoli and expiration becomes difficult.
Air trapped in alveoli causes hyperinflation (Barnett 2006)which damages the structure of the alveoli.
Hyperinflation of the alveoli causes deterioration to the elastic fibres (barnett 2006).
This breakdown in elastic fibres leads/progresses to emphysema or at least contributes to the onset of the disease.
Periodic obstruction generally becomes permanent, air can no longer reach the capillary bed in alveoli due to blockage so no gaseous exchange can occur.
This leads to hypoxia and hyper-capnia in the sufferer.