COPD
Contact Us: 07957266649
Chronic
Obstructive
Pulmanory
Disorder
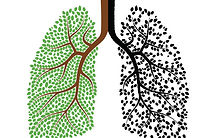
information for patients on COPD
Diagnosis of COPD
Diagnosis strategies
-
patient medical history
-
physical examination
-
spirometry measurements
-
radiologic studies
Patient's medical history
Often a patient can live with one or more symptoms of COPD such as chronic cough or shortness of breath for quite some time allowing the ailment to develop without any treatment strategies (Haas & Haas 2000). this is why it is important to check the patients' medical history to uncover if they lead a lifestyle that is associated with and can lead to COPD.
This medical history check involves looking into these following factors
-
history check includes
-
smoking's habits
-
environment with attention to occupational exposure
-
dyspnoea
-
coughing
-
wheezing
-
acute respiratory infections
Physical examination
There are a number of physical symptoms that will manifest in sufferers of COPD, a physical examination will assist in acquiring further information about the patients' health, and assessing whether they have or at what stage there chronic obstructinve pulmonary disorder is a these various examinations include
-
Checking skin colour for cyanosis particularly around the lips.
-
Checking finger tips for finger clubbing & cyanosis.
-
Check jugular venous pressure which may be high in advanced COPD due to cor pulmonale.
-
Check for peripheral oedema which is commonly evident in patients with severe COPD.
-
Check chest inflation, poor chest inflation can be a sign of hyperinflation in the lungs.
-
An Audible and visual examination of the chest wall and back will be performed. Audible sounds will differ from lungs with bullae to normal alveolar sacs; also the presence of excess mucus is also detectable with a stethoscope.
-
Audible examination of breathing noises in an attempt to hear obstructions. (Barnett 2006)
spirometrey measurements
Once COPD is suspected on clinical grounds, spirometry is the best method for accurately assessing airflow obstruction(Barnett 2006). The patient is asked to forcibly exhale until there is nothing left to expel after a full inspiration.
This measures the patients forced expire try volume in one second (fev1) which is the volume of air that can be forcibly exhaled in the first second of forced expiration after maximal inspiration.
And also the forced vital capacity (FVC) which is the maximum volume of air that can be forcibly exhaled from maximum inhalation to maximum exhalation (residual volume) measured against time.
and RVC (relaxed vital capacity) is a non-forced expiration measurement, which is often greater than the FVC in patients with COPD.
These measurements are used to obtain whether the patient has an airflow obstruction FVC1/FVC should be over 80% in healthy unobstructed lungs (Barnett 2006). COPD can be diagnosed as mild, moderate or severe depending on the level of fev1 compared to the reference values of a person of similar age sex weight and height.
Radiologic studies
Radiological diagnostics such as x-ray can be used to exclude alternative diagnosis in the early stages of COPD, in the later stages of COPD radiological changes picked up by x-ray or CT scan include enlarged lungs due to air trapping (Price David, Foster Juliet, Scullion Jane, Freeman Daryl 2004), also an right side hypertrophic heart will be visible in later stages due to cor-pulmonal (Price David, Foster Juliet, Scullion Jane, Freeman Daryl 2004).
Treatments
non-pharmacological
Quit smoking
Cessation from smoking can help slow down the decline in lung function (Bourbeau, Nault & Borycki 2002). Smoking is the main cause of COPD and therefore quitting smoking can slows down lung decline compared to those that don’t stop smoke.
Importance of exercise
Exercise even if minimal can help keep the lungs healthy by improving lung capacity & exercise tolerance (Bourbeau, Nault & Borycki 2002). Even damaged lungs from COPD are capable of exercise (within limitations) although breathlessness is distressing it is not harmful. Patients with COPD however often gradually stop exercising due ot the degree of breathlessness they experience. As a result of this there is a danger of patients entering a spiral of inactivity which leads to further mobility issues, increased dependence & a lower quality of life. Regular exercise is vital to lead as normal a life as possible.
Oxygen therapy
Oxygen therapy is used in patients with severe COPD who become hypoxemic, Although oxygen therapy doesn’t stop the feeling of breathlessness it does help reduce some of the other complications of COPD (Bourbeau, Nault & Borycki 2002) such as cor pulmonale, polycythatemia and peripheral odeama . it does thos by raising the percentage of oxygen in the air that the patient breaths therefore increasing the users sp02. Oxygen therapy is delivered through a nasal cannula.
Although COPD has no cure (Barnett 2006) there are various pharmalogical and non-pharmalogical options to manage COPD.
The goals of the treatments are too;
-
To slow the progression of the disease
-
To limit symptoms such as shortness of breath
-
Increase the patients overall fitness, mobility and independence
-
Prevent and treat exacerbations
pharmacological
Bronchodilators are the primary drug therapy of those who suffer with COPD there are three types of bronchodilator including inhaled beta-2 antagonists, anticholinergic and oral theophylliens.
Beta-2 antagonists act directly on bronchial smooth muscle to cause bronchodilation ( Simonds , Muir & Pierson 1996). This includes drugs such as salbutamol and terbutaline.
Anticholinergic drugs act by inhibiting resting broncho motor tone (Simonds, Muir & Pierson 1996), by blocking the bronchoconstictor effect exerted by cholinergic nerves within the lungs. This includes drugs such as ipratropium bromide and tiotropium bromide.
Both of these types of drug affect the degree of breathlessness the patient suffers with, they can also help reduce air trapping which increases tolerance to exercise.
These drugs are usually administered in short acting and long acting doses. Short acting doses are stronger doses of the drug commonly used for a rapid onset when symptoms such as breathlessness flair up these are used as a relief drug (Barnett 2006). Long acting doses are weaker and have a longer onset of action and also a longer duration of effect so these can be taken routinely to minimise symptoms (barnett 2006).
Theophylline is used to relieve the symptoms of breathlessness, only used when other inhaled bronchodialators have been optimised (williams 1993). Their mode of action includes relaxation of smooth muscle in the airways the mechanism however is unknown (vassallo and lipsky 1998) this improves ventilation. Theophylline also has effects on mucociliary clearance which also aids in improving airflow (Haas & haas 2000) . Also the drug is known to improve cardiac output which can be valuable in patients suffering from cor-pulmonale (Rosen , Sharma & Oakley2004).